Air resistance: COVID
CIRES/CU-Boulder-led study: Why it took so long to recognize airborne transmission of the coronavirus, and how to do better next time

Millions of people died of coronavirus infection because institutions and people took too long to recognize that it was primarily airborne, and a new study traces that deadly resistance a hundred years back in history, to the rejection of sickly air called “miasma,” the rise of germ theory and our own stubborn tendency to retain beliefs in spite of accumulating evidence to the contrary.
While SARS-CoV-2 viruses were invisibly infecting people in 2020 through the air in hospitals and churches, workplaces and restaurants, we were busy disinfecting surfaces and groceries and washing our hands. We installed plexiglass walls that actually increased coronavirus spread, said Jose-Luis Jimenez, lead author of a comprehensive new assessment of major medical mistakes involving respiratory diseases, just published in the journal Indoor Air.
“History set us up for a poor response to the pandemic,” said Jimenez, a CIRES fellow and distinguished professor of chemistry at CU Boulder. “We might have had millions of fewer deaths, hundreds of millions fewer cases, if we’d taken appropriate, effective action from the start.”
The overview, written with colleagues from 10 countries, illuminates the often deadly impact of “belief perseverance,” in which it can take years, or decades to challenge a set of beliefs—especially when the consequence of changing a set of beliefs is costly. It’s less expensive to ask people to wash hands or disinfect surfaces than it is to update a ventilation system, for example, or to re-engineer school classrooms, city buses and corporate boardrooms.
The authors, who include physicians, virologists, public health specialists, aerosol scientists, engineers, historians, a sociologist and an architect, spin through numerous examples of fatal mistakes in the history of research on infectious diseases. In 1847, for example, a scientist working in Austria showed that handwashing by medical doctors reduced deadly puerperal fever in a clinic. His work was dismissed because at the time, established medical and scientific beliefs blamed “a miasma in the air.” Handwashing made no sense to the establishment, and the suggestion that physicians, themselves, might be spreading disease, offended many.
Half a century later, another prominent researcher, Charles Chapin, ridiculed the idea of spooky miasmas or infected air. Chapin’s own work on infection had suggested to him that “contact infection” was the predominant way most infections spread. But he was also savvy about how difficult it was to persuade people to wash their hands and disinfect surfaces if they thought some diseases might spread through the air, and how difficult it would be to figure out how to clean the air itself. So he argued without evidence and managed to effectively label airborne disease transmission as superstition.
Jimenez and his co-authors trace history from Chapin to 2020, when the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC) and other institutions expressed deep skepticism or outright denial that SARS-CoV-2 might spread through the air, despite increasing evidence it was doing just that.
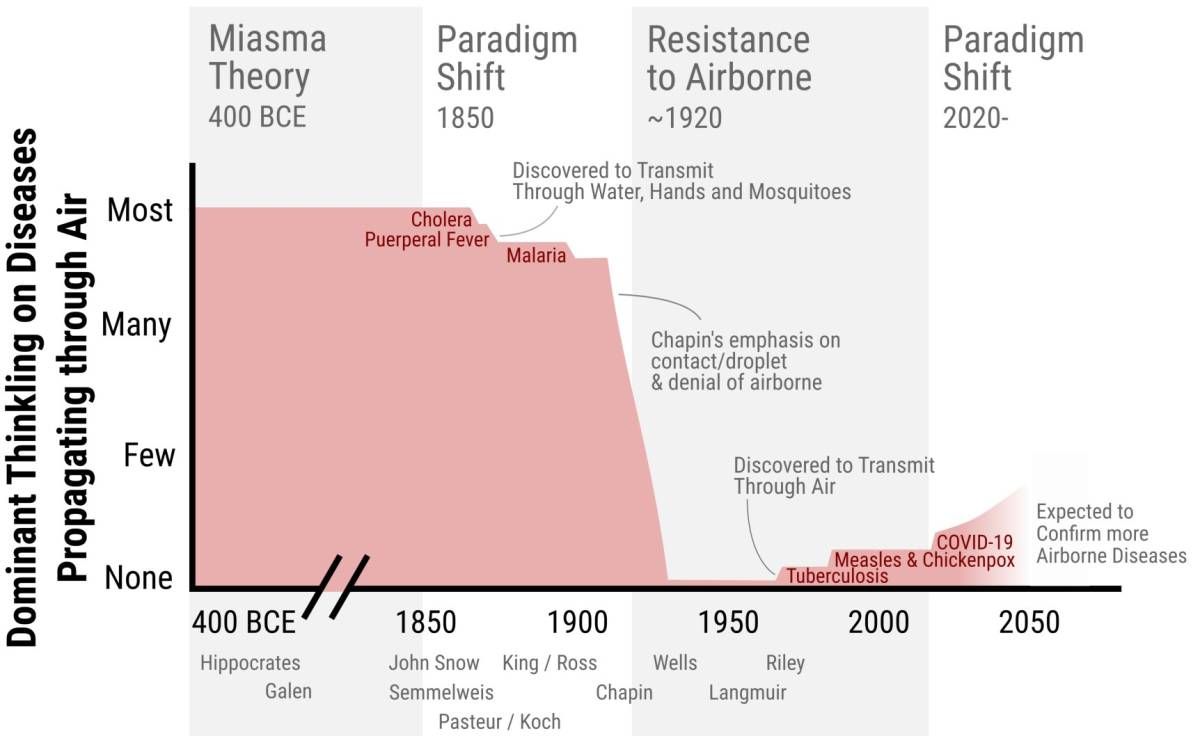
FIGURE WHICH ILLUSTRATES THE DOMINANT MEDICAL AND PUBLIC HEALTH THINKING IN THE WEST ABOUT HOW MANY IMPORTANT DISEASES TRANSMIT THROUGH THE AIR.
Jimenez said he thinks that most people at WHO and CDC were honest in their skepticism in early 2020, just struggling to get their minds around the fact that the conventional way of thinking about respiratory infection transmission—spreading through heavy droplets falling on surfaces—might be inadequate to explain the pandemic. “They were stuck on the theory, distorting the interpretation of the observations to match their pre-existing beliefs,” he said.
Others have suggested that economics have also been at play, much as with climate change. It’s convenient to ask individuals to take small, individual actions like handwashing and driving less, Jimenez noted. It’s more expensive for institutions to make structural changes, such as increasing ventilation everywhere, or replacing fossil fuel infrastructure with renewable energy.
So in preparation for facing the next pandemic intelligently, Jimenez said, he and his colleagues are first working to find allies, especially in the hardworking medical and public health professions where many people have been too busy saving lives to enter the discussion about disease transmission, but have direct experience.
“And confrontation is also needed when major institutions refuse to accept the science and to communicate it clearly,” Jimenez added. “Maybe we have to badger the establishment a little, like Florence Nightingale did.” Nightingale “lobbied” the British government for decades to support her reforms at hospitals, increasing hygiene, ventilation and distance between beds at a time when it was still seen as unnecessary.